TORONTO -- One of the scary things for doctors about treating COVID-19 patients is they can appear stable one minute, then deteriorate quickly with sudden drops in oxygen levels that could kill them.
Keeping an eye on these patients has been a challenge for front-line teams -- especially since the patients are often in rooms with closed doors because of their infectivity.
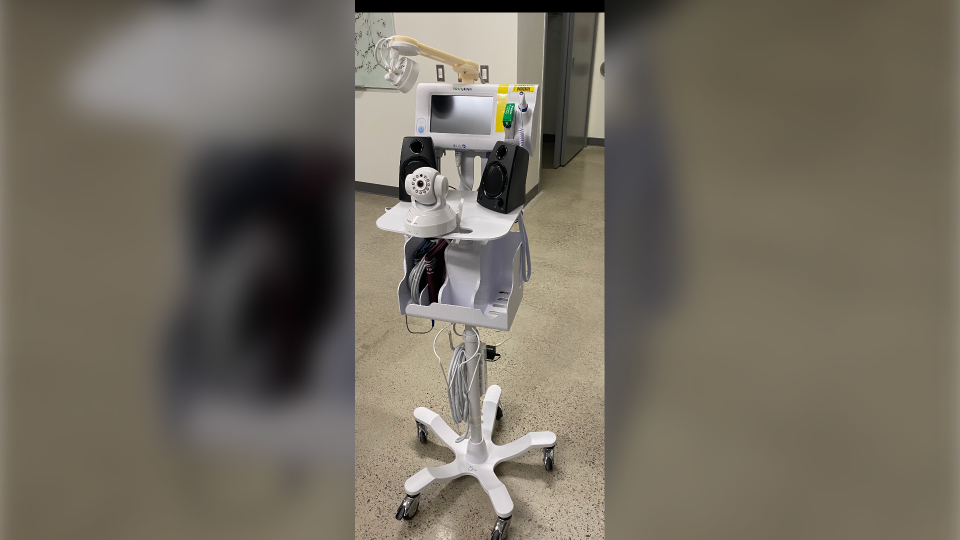
Now a team at Toronto’s University Health Network (UHN) has designed a system that will monitor these "fragile" cases using a telemonitoring system, which may become a standard of care in the COVID-19-era when patients are often isolated.
"The benefit of the patient is: one, better monitoring; two, is less social isolation; and also security, like they don't feel so scared and alone," said Dr. Shaf Keshavjee, Surgeon-in-Chief, Sprott Department of Surgery at UHN.
Some hospitals in the U.S. have turned to baby monitors to communicate with patients and prevent unnecessary visits to inside the rooms of COVID-19-postive patients -- primarily so that gloves and masks aren't overused in light of the shortage.
The new Canadian-designed system uses two cameras, one facing the patient, the other pointed at the machine showing blood pressure and oxygen saturation. It's connected to a system where technicians can monitor six to seven patients at a time, often from floors away.
The system is also equipped with two-way audio communication so the technicians and nurses can speak to the patient, and the patient can call on them, without requiring them to put on personal protective equipment (PPE) for a short trip to the patient’s bedside.
And a key benefit for COVID-19 cases: it can monitor oxygen levels and send out an alert if they drop.
"The technician can check. Is it just a little change in the saturation because the patient moved? Or is it because a patient pulled their oxygen mask off, and they can just tell the patient to put the oxygen mask back on?” said Keshavjee. “And in this way it avoids the nurse going back in the room, and having to be exposed to COVID but also wasting PPE every time they go in and out of the room."
If the patient is having a serious drop in oxygen, linked to worsening COVID-19 disease, they can be quickly transported to the ICU for further treatment.
The system is the brainchild of nurse practitioner Marijana Zubrinic, who has worked in the thoracic unit at UHN for nearly a decade.
Originally designed for lung surgery patients who rely on oxygen masks, it went officially on line at Toronto General, Princess Margaret and Toronto Western in August of 2019. Early data showed it improved efficiencies -- the hospital didn't have to hire "sitters," people who were assigned to sit in the room with fragile and often delirious patients to make sure they stayed in bed and kept their oxygen masks on.
It also reduced the workload on nurses. If a monitor or sitter wasn’t assigned, nurses might need to drop in on patients up to 20 times a shift to remind them to stay safely in bed or keep their oxygen in place. The visits dropped to three-to-four per shift as remote telemonitoring allowed technicians to intervene first with audio reminders. Patients could also ask for the nurses to visit if needed.
But then came COVID-19.
Fragile patients could no longer have a sitter in the room, while gowns and masks and gloves also became critical resources in short supply.
"We wanted to prevent any unnecessary exposure to the nurses," says Zubrinic. "It's unnecessary to go into a room with full PPE to put the oxygen probe back on if the patient can do it themselves with a reminder."
The system also gives nurses a tablet that allows them to talk directly to patients and access a camera to zoom in on faces and vitals monitors.
Brittany Cole, a nurse at UHN who used the system on a COVID-19 patient recently, said she “loved it."
“I am a big fan,” she told CTV News by phone.
"We got a call from the telemonitoring (desk) that a patient (who was later confirmed as COVID-positive) took off the nasal prongs and the oxygen levels were dropping. Within a minute of calling us ….we got to the patient's room. It saved it from turning into a bad situation and (the patient) deteriorating quickly."
The feedback from patients in the initial trial in the lung unit was positive, said Zubrinic.
"Patients find it reassuring,” she said. Instead of finding it an intrusion on their privacy they, say “it’s an extra set of eyes to keep me safe," she added.
With COVID-19 patients now a fixture in hospitals for some time, other hospitals are approaching UHN for information on the telemonitoring system.